Our healthcare politicians and leaders are sitting on a simple and exquisite opportunity that isn’t hard or expensive, would transform patient experience, and would save billions. But they can’t get on page.
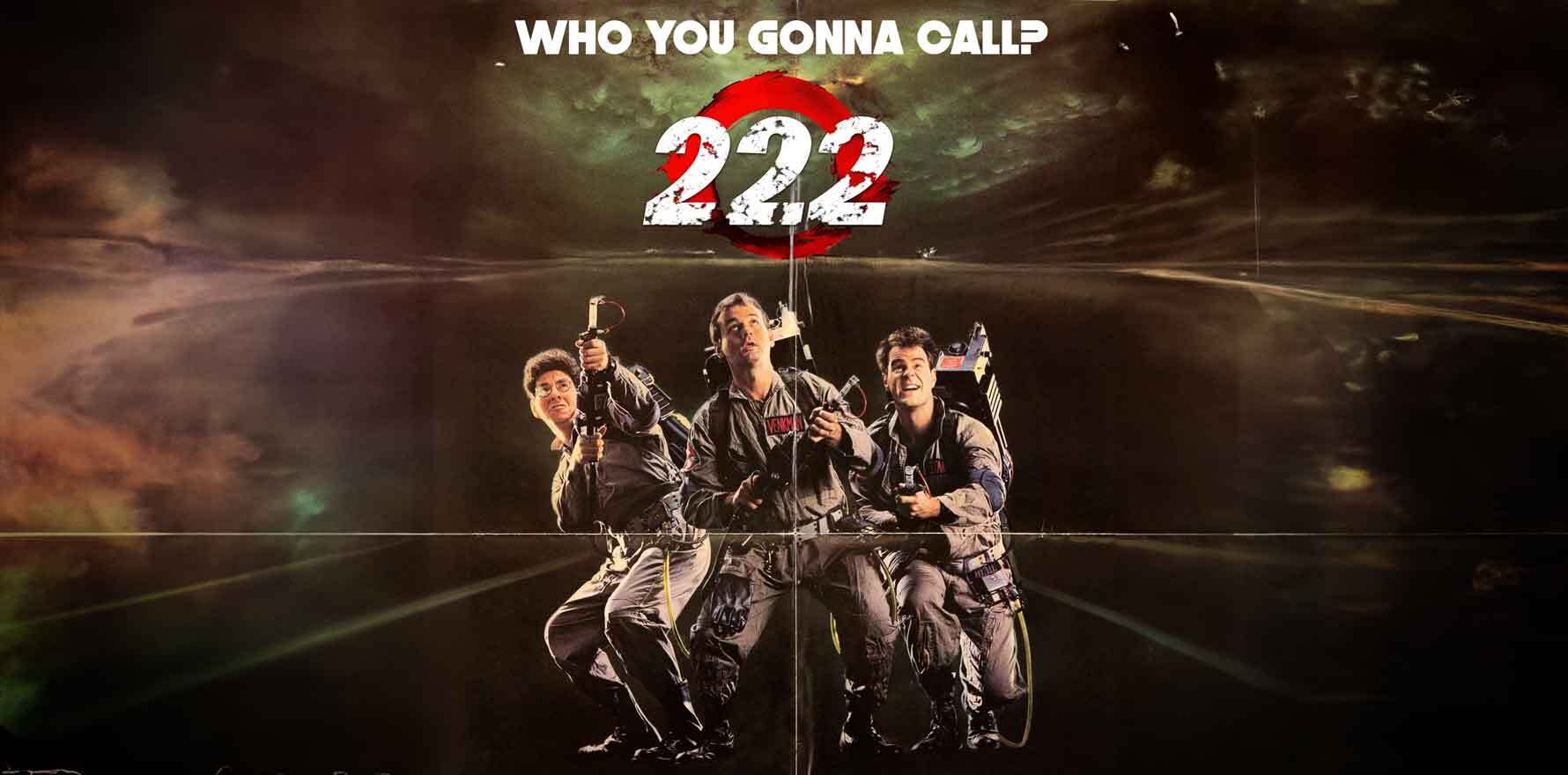
A few weeks ago I wrote about the idea of 222, as discussed by two key healthcare leaders from Victoria and NSW at a recent digital health gathering.
The idea is simple: have a universally recognised number – other than 000 – that would, through well researched and developed algorithms and emerging cloud and AI technology, direct patients with non-life-threatening conditions to every other point of the compass in our healthcare system with relative accuracy, speed and ease.
I got inundated with feedback, most of it in support of the concept, some of it adding some important information and political colour to the story which I want to go through now. The idea seems like a very rare opportunity to move the dial on our wickedly complex healthcare system without too much money or effort.
A lot of people wonder why the idea of 222 hasn’t been seized upon by both state and federal governments as an initiative that so obviously will save the system billions, and transform the lives of all sorts of patients – after-hours worried mums (and dads), aged care nurses on shift worried about what to do, GP patients who aren’t quite sure it’s a GP they need, or who can’t get to one in time for an urgent antiviral, or urgent mental health helpseekers completely confused by the many choices on offer today. And so on, all across the country.
The idea in its simplest form is that if you as a patient know you don’t need an ambulance, but after that you aren’t quite sure what you need or how to get to a particular service that you think you need, you call 222.
When you ring 222 you start a journey that some people are loosely giving the term “single digital front door”. A phone number isn’t technically digital, but any 222 number will obviously have a digital app component to it if it gets up properly.
I say “loosely” because for a definition which has the word “single” in it, it’s not exactly singular in the way our federated and highly politicised healthcare system is treating it.
We already have scores of SDFDs or lookalikes around the country, and sometimes we have many within regions within states.
Depending where you are and what you are thinking you might need you might be faced with deciphering an average up to 10 phone numbers or, usually 1800 or 1300 numbers (which no one remembers anyway) and if you are thinking you’ll go online, you will likely face a lot more confusion – particularly if you’re seeking advice on mental health.
In some respects this problem exists because we have a highly fragmented system and patient experience.
But 222, done right, would take this problem away from the patient. They just ring 222 and go from there.
It would also save the system billions in a very short space of time.
Ironically, one problem that seems to have emerged about this idea (which leads to one of many objections to the idea) is that it’s too simplistic.
Certain groups feel that their expertise in managing, say, a mental health patient, will get delayed, diluted, or even missed by making everyone go to one number first.
It’s an understandable misunderstanding about the concept, but it is a misunderstanding.
Dialling 222 is a single doorway in the true sense. It’s one universal entry point. But it’s an entry to a highly sophisticated and researched set of algorithms sitting underneath which, done properly, will end up in significantly more people getting to the right service they need much faster than they would have otherwise.
It won’t only save money, it will undoubtably save lives in the end.
A 222 call is the start of highly sophisticated triage, enabled significantly today by cloud-based call centre technologies, and, yes – I hate to say it – AI.
Once you call 222, you are entering a world where the maze of your correct healthcare options are managed for you by real people assisted by sophisticated algorithms to assess where you really should go and how you get there in the fastest way.
The 222 call will be a piece of infrastructure managed by one organisation and as such it will be a central corralling and learning point for the whole country. What works in a remote region of WA may well be an algorithm that can be easily applied to western Queensland with great effect.
It should end up as a growing and invaluable pool of regionalised population data. It will also avoid the reinvention of different wheels independently all over the country, with the awful waste that results in, and which we already see a lot in our federated system.
A 222 call will be farthest thing from one of the most common misunderstandings about it: that only having one number will herd too many people with too many problems to one place that can’t possibly manage the complexity.
It’s the opposite.
The 222 call is just the front door. Behind it is a mass of living, evolving data and IP about the system, its regions and the specific needs of patients within those regions. It’s a connector to a complex web of region-by-region health providers. With AI it will foster living and constantly evolving algorithms which will be able to take into account elements of a patient’s situation and needs that the literally hundreds of numbers we have today can’t ever hope to do.
Key components will include things like regional population health trends, socioeconomic factors, all the local health provider services and their accessibility by time and sometimes even by capacity (hospitals, pharmacists, GPs, specialists, mental health services and other allied health where possible) and more.
As 222 evolves, more and more data from the patients using it will finetune it, in part using AI (of course).
Let’s just take this idea and compare it for a second to some of the things that are currently happening in our system, to make some rough comparisons as to the value that could be created here to how we like to run things now.
Today we have lots of versions and interpretations of SDFDs, state by state, and even region by region.
To name a few:
- South Australia is developing their own version of an SDFD, but not for every health service and not every region yet;
- Victoria has a version of an SDFD for emergencies (which is triaging where it can to virtual to save the system the money of physical attendance at EDs);
- an SDFD that looks like a true state version of what is being pitched here is being developed for the whole of NSW (its not up yet);
- NSW has just decided to add all mental health services to its supposed SDFD, which suggests they still don’t get the full potential and scope of SDFD because mental health should have been in scope day one. It probably means a whole lot of stuff is still out of scope in our most interesting emerging pilot for the 222 concept;
- many of our PHNs, some in NSW even – the state clearly doing one SDFD – are doing their own local version of an SDFD, which is verging on the bizarre because they don’t have ongoing funding, they often aren’t connected well enough to GPs in their area to make it work, and they don’t have the massive advertising and marketing budgets to make the idea work locally either;
- and so on … if you go state by state you can find a lot of versions of the idea, but all of them are being developed along the lines of “if it wasn’t built here we don’t think it will work” (it’s a version of NIMBY).
Into this mix you can throw the state and federal governments’ urgent care centre programs, and the advertising and promotion around each, all with a different starting point digitally and on the phone, a myriad of mental health numbers – Head to Health distributed among various PHNs and federally, Beyond Blue, Lifeline, Headspace – and any number of other well-meaning but hard to get to and understand services locally (eg, Men’s Shed).
And we haven’t even talked about aged care.
You might already be thinking you know what is wrong here, outside of “not invented in my backyard” syndrome.
If someone says “okay everyone, if people aren’t ringing 000 they are ringing 222” there is an immediate (and understandable) fear among all these organisations that they lose control (and with that probably to some extent power) of their distribution and therefore their organisations.
Correctly run, the opposite is true of 222.
The only problem some of these organisations might have is that they may not end up getting patients who they should never have gotten in the first place. And that is a fear that the politicians should stare down with these organisations for obvious reasons.
Let’s take a quick random example of a patient and compare the processes here.
Joanne Bloe, a single mum in a small northern rivers town is hugely stressed because her home got flooded recently and she is living with her two young children in temporary accommodation. One child is sick with a fever at 9pm on Saturday, after she’s had a few drinks to relax for a quick break at the local bowlo.
She’s really worried but not sure she needs an ambulance and is thinking she might get charged for it if she rings them.
Who’s she gonna call?
In her small local town there does happen to be a GP but she got on Hotdoc and there isn’t an appointment until the following Tuesday.
She’s on the web looking for options. She sees an ad for 13SICK after hours but they don’t service the region.
There’s a late-night chemist in the next town but she can’t drive there and she rings and no one answers – it’s Saturday night.
After a bit more internet work – luckily the local internet got restored after the floods a couple of weeks ago – she finds HealthDirect.
HealthDirect is a not-for-profit group specifically funded by every state and territory government and the federal government to do … well, to pretty much do as close as they can to 222. Go figure.
She rings them. She gets triaged by a nurse, who works out that one of the two common household pain medications would probably do the trick in the right dose, and advises the poor mum that if this course of action doesn’t get anywhere, then to ring back and she could arrange a virtual GP visit as a next step.
That eventual step for this patient’s mum saved a lot of heartache, stress and probably money, both for the patient and the system.
It’s not a coincidence that of all the organisations in Australia that are pursuing the idea of 222, and who have a fairly sophisticated service in play already, HealthDirect is the “most likely” organisation to pursue the idea properly.
Fun fact. HealthDirect’s phone number turns out to be 1800 022 222.
True story: I was having a Zoom call with HealthDirect the other day, not even remembering who first hinted to me that 222 would be a great number for the ultimate SDFD for Australia, and everyone on the call at one point admitted if they’d ever used the service. I said that in the last six months, with a mum in aged care and a partner who got shingles (and RSV) and needed an antiviral ASAP I would have rung them in a heartbeat, but I couldn’t remember the number.
To be honest, HealthDirect, although I know it well, wasn’t to me that big a brand so it has never much been top of mind.
That is probably not HealthDirect’s fault for the most part. You need all governments to agree on how the organisation is promoted and it needs to be clear and uniform and you’d probably need money HealthDirect hasn’t got in terms of promotion.
I would certainly have remembered 222. No need to have seen advertising about HealthDirect and what it offers anywhere – 222 is a killer brand.
It must be, I tried to buy 222.com.au on GoDaddy and they wanted $23,402.50. I’m sure DoHAC can afford it if it comes to that.
My journey when I failed to recall the HealthDirect brand (and no 222 was available), as a typical reasonably affluent patient turned out to be pretty tortuous one to get that anti-viral.
It started on a Friday afternoon on the northern beaches of Sydney. Wealthy right? And more GPs than you can poke a stick at, with a punter who was prepared to pay top dollar to get in quickly so he could get his very sick and quickly getting sicker partner into the 24-hour anti-viral window.
Do you think I could find any GP within the whole region after 3pm on a Friday? Not a chance.
After attending two walk-in GP centres that advertised themselves as only walk-in and which were full to the brim, I did the thing I most dreaded but felt I had no option. We went to Northern Beaches Hospital.
There’s a lot of bad press about Northern Beaches Hospital but it’s not the people at the hospital that are the problem. It’s the people funding it.
After five hours, with no information on when we might be seen, and my partner with severe aches and pains, we abandoned that idea. I should have known – the last time we had tried we left after we got a ticket with the number 47 on it.
We got rung up two hours later by a panicked resident who said come back. They probably took that long to get to the notes and thought, shit, this person could actually be pretty sick.
She was. RSV of course is highly infectious.
You’d think I’d know how to work this problem out better. Yes, there were other options that were easier that a lot of readers will be thinking I should have have known about, but when you’re stressed and it’s family you don’t tend to think in a straight line.
Turns out that if I had remembered the HealthDirect number and understood that my partner could get prescribed antivirals for shingles on a virtual telehealth call, I could have solved that problem at 3.05pm on Friday.
But I didn’t. We had a terrible weekend. We managed to find a GP in Sydney on Saturday at 11.30pm.
Who in the world of federal and state politics, and all the regional health politics that cascades below this system level, are holding out against this idea and why?
Because there are quite a few.
There’s one category I’m going to dismiss immediately, and leave it to my faith in state and federal healthcare leaders to deal with – those many organisations who fear that 222 – that one step in between them and a patient that will need to be added – will take away control.
It simply won’t. It will finetune the system to make sure that the patients get the right service much faster, plain and simple.
One problem groups that run this line have is that they actually don’t run the line at all. They say something else because they know running that line is going to get stomped on. But that they come up with a whole lot of other reasons not to participate or to develop a local solution isn’t helping. Most of them should be dealt with by health leaders who are prepared to put their foot down.
If we can trust the powers that be to filter all this obviously dysfunctional stuff out, we seem to be left with just a few final problems.
One is the idea that “no door is a bad door”. This is apparently a strongly supported idea in Victoria, a state with 82 hospital districts effectively, so presumably lots and lots of non-bad doors.
For some reason, the idea is being seen as an argument against a real single digital front door – 222.
But the two ideas are perfectly synergistic.
In healthcare, the idea is to get to the right door. The door that perfectly matches what you need as a patient and what is most effective from a system economics point of view.
The big trick is getting to that door. The whole idea of a properly run 222 infrastructure is that people get to right door.
“No door is the wrong door” is not an argument against 222. It’s an argument for it.
If you want to get to the right door, call the organisation with the most IP, the most sophisticated call centre and cloud technology, the most AI and the most universal co-operation between the states and the regions, to get you to that door. An organisation which runs 222.
Maybe we have one political problem left here, I don’t know.
Who runs 222?
It feels like it shouldn’t be a problem.
HealthDirect is funded by and reports to every state and territory and the federal government to do, mostly, what the concept of 222 is all about. It’s already well on its way on a trial in the biggest state in Australia, NSW.
And, since covid, it has sharpened its reason for being a lot – it was getting confused for a while until covid gave it a very well-defined purpose – and it now has the management and the technical capability to build and run such an important and ambitious project.
Some hospital folks high up – the same folk who ultimately fund HealthDirect – put it about that HealthDirect was being way too conservative in their triage algorithm today and sending too many people to hospital EDs unnecessarily. I am reading “safety conscious” for conservative here which we should all be glad for.
That’s some pretty bizarre political logic. We fund you to triage but we don’t want anyone to know about you because we think you triage badly.
I haven’t gotten to the bottom of the data and evidence for such a claim. It feels a bit spurious, even Trump-like, in its construction.
But just say HealthDirect is triaging badly (not just being highly safety conscious and developing good compliance). Then fix it. You’re funding it, right?
And how would you fix it?
By doing the 222 project which would provide you with all the data you’d need across the whole country to prove the criticism out one way or the other. And make sure it wasn’t happening.
In any case, what does a state hospital administrator think would happen to that patient who unnecessarily came to their ED if they didn’t have HealthDirect to call? Magically find the right healthcare door they needed themselves?
As my experience proves, we consumers are pretty uneducated and stupid in navigating what is already a highly fragmented and confusing healthcare system.
At the end of the day, this argument is more control politics, which the health leaders need to recognise, and step through.
So, what do we do now?