The votes are in. ‘The health system does not enable and support [healthcare professionals] to consistently deliver the care that is within their skills, training and experience’. So, what now?
The long-awaited scope of practice review has arrived, outlining an “ambitious program” of reforms.
While the federal health minister, Mark Butler, seems onside, does he have the gumption to face “turf wars” and “political fights” to enact implementation?
Last August saw the inauguration of the Unleashing the potential of our health workforce – scope of practice review.
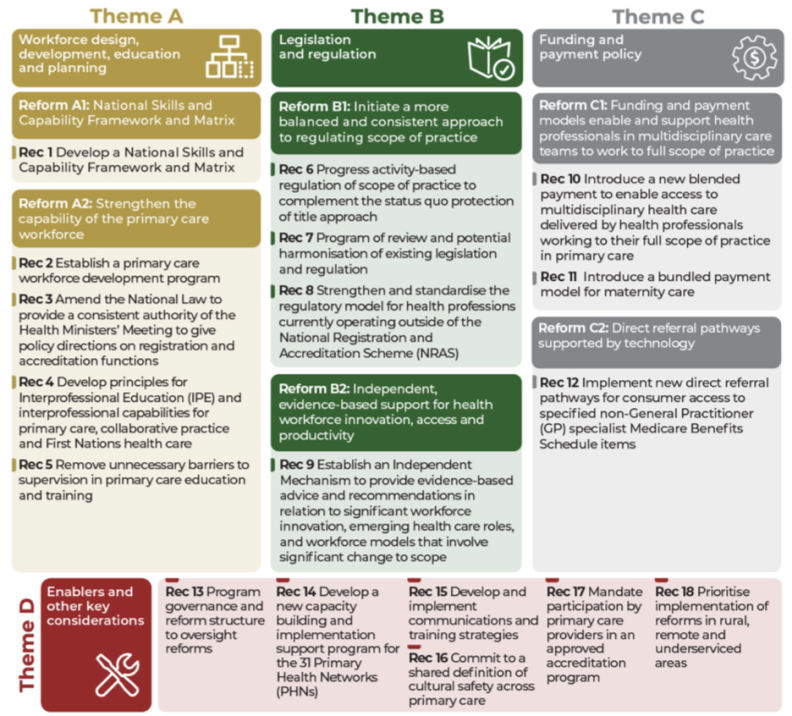
Today, lead reviewer Professor Mark Cormack and his team released the review’s final report, including 18 recommendations.
The report reiterated many of the suggestions of its predecessors – issues papers one and two – namely that health professionals are being held back from working at their full scope by a range of unnecessary barriers.
“The review found that virtually all health professions in the primary care sector, including general practitioners, face some restrictions or barriers to working at full scope of practice that are unrelated to their education (skills and knowledge) and competence,” reads the final report.
“These barriers were noted to shape the primary care workforce and influence sustainability of the workforce over time, particularly in rural and remote locations.”
According to Mr Butler, this validated the frustrations of much of the healthcare workforce.
“The health system does not enable and support [healthcare professionals] to consistently deliver the care that is within their skills, training and experience,” he said.
“This is not a case of a single profession missing out. The review tells us that virtually all health professions are held back by restrictions and barriers that are unrelated to their skills, training and experience.
“Removing these barriers would make it easier for Australians to get high quality health care, when and where they need it, without waiting weeks or driving long distances.”
When asked about his appetite for change on ABC AM, Mr Butler said he was “very determined” to remove any “artificial, inefficient restrictions” to scope, “along with improving the digital capability of a system that uses still far too many fax machines and too much paper”.
“This is a really important reform opportunity, because, at a time where demand for health is growing and will grow, as long as I can see into the future, and workforce is hard to come by, it just doesn’t make sense not to use every skerrick of skills and training that all of our health professionals have, from GPs through to nurses through to pharmacists, physios and more,” he said.
When asked if he had the “gumption” to face the slew of “political fights” coming his way if he intended to enact change, Mr Butler said change was already underway.
“Last week we made change for nurse practitioners and endorsed midwives,” he said.
“We got rid of the old restriction that required them to be working in collaboration with a doctor, effectively having a doctor look over their shoulder as they went about their very, very skilled work.
“We’re already making change in this area, but this report makes really clear just how much opportunity there is to unleash the full skills and training of the best trained health workforce on the planet.”
Mr Butler acknowledged the “turf wars” in healthcare.
“At its worst, frankly, I think sometimes this sector reminds me of factories back in the 1970s with very strict demarcations,” he said.
“We were able to break them down, get much more efficiency into manufacturing, and much more value and reward for the workers involved.”
The report’s 18 recommendations sat across four themes: workforce design, legislation and regulation, funding and payment, and enabler and other considerations.
The review found that interstate/territory inconsistencies hampered health provision, particularly rurally and regionally, and should be removed.
“Many of the recommendations will require collaboration between the Commonwealth and state and territory governments, as well as consultation with peak professional organisations, AHPRA, patient groups, and the sector more broadly,” said Mr Butler.
Mr Butler said he wouldn’t talk to each recommendation individually but said “a lot of them do have a lot of common sense”.
He noted, in particular, recommendation 12 calling for direct referrals to non-GP specialists, circumventing the need to return to a GP.
The recommendation has been met with indignation from GPs.
But Mr Butler insisted it was in their interest.
“I think it’s important that GPs are kept in the loop and that goes to that question of digital connection, so that the GP knows the psychologist has referred their patient to a psychiatrist,” he said.
“There are all sorts of inefficiencies that mean that a lot of precious time of our GPs is being soaked up through these sort of back and forth of referrals.”
Speaking to Health Services Daily, The Australian College of Nursing National Director of Professional Practice Karen Grace said the most important finding for the college was the “public acknowledgement of the limitations to public health professionals to work to their full scope”.
“It’s tricky to pick the most important [recommendation] but for the nursing profession, the blended funding models will be a huge win in terms of enabling us to introduce and scale up more nurse-led and team-based models of care, where nurses are actually supported to work to their full scope.
“At the moment, under existing Medicare funding models, it can be really problematic for nurse-led and interdisciplinary models of care to effectively remunerate every healthcare professional that’s part of the team that’s providing care, which limits the scope of some of those programs.”
Mr Butler told ABC AM that the government was already looking into blended funding models.
“You see that overseas quite a lot and it will take time,” he said.
“This report makes clear there’s a very long runway that will be needed to move to a system like that.
“We’re right now trying some areas where that might work for, example, older patients in residential aged care and we’ll look at that recommendation very closely.”
Ms Grace said it seemed there was appetite for serious reform from the Commonwealth government.
“This report describes serious and significant reform in the primary care space for healthcare provision, there’s a whole range of recommendations that sound simple on paper, but will be incredibly complex to implement.”
Ms Grace said recommendation nine – establishment of independent mechanisms to provide evidence-based advice in relation to workforce innovation – would be pivotal to the workforce.
“That speaks to development of innovative models of care that work to the scope of all the health professionals within the team, including nurses,” she said.
“Those models would need to be supported through blended funding models, because the current funding structure wouldn’t be fit for purpose at this point in time.
“On top of that, there’s a whole range of regulatory and legislative barriers that need to be addressed, particularly in relation to differences in in legislation between jurisdictions.”
The college also called for national implementation of a “competency passport” to allow the workforce to carry proof of competency beyond the minimum job requirements from job to job.
The Australian Physiotherapy Association also welcomed the report.
APA national president Scott Willis said the report offered the structural reform necessary to improve care and collaboration.
“APA welcomes the proposed shift towards a blended payment model, a much-needed step for equitable funding that supports multidisciplinary teams in delivering high-quality, patient-centred care,” he said.
“Australia is embarking on a nationally significant reform journey. We’re closer than we’ve ever been but with another electoral cycle approaching, the path ahead remains pivotal.
“However, given the scale and complexity of the issues, we should not expect huge change overnight.”



