It’s called ‘whole-of-life product support’ and it makes no sense we don’t have it for human beings.
All manufacturers have to service and repair their product over its lifetime. Car manufacturers allocate funds to cover their five-year warranties and have whole-of-life product support for 10 to 15 years.
Famously you can buy brand new Mercedes parts from the cars that were manufactured back in the 1960s and the 1970s. Their website says: “From the smallest washer to an entire carburettor assembly, Mercedes-Benz continues to manufacture spare parts that support our heritage models”.
Car companies have a 25-year business planning horizon. I can’t find proof, but it is rumoured that Toyota has a 100-year business plan. The interesting thing is the business plan is longer than the lifecycle of the product.
In Australia we are manufacturing 300,000 new products a year, and by that, I mean human beings – 300,000 is roughly the number of births in 2023.
It is predicted that males born today will live to about 81 years and females about 85 years. So, you would think based on the principles of good product lifecycle planning we would have a 100-year health pan.
Good luck finding (and funding) one.
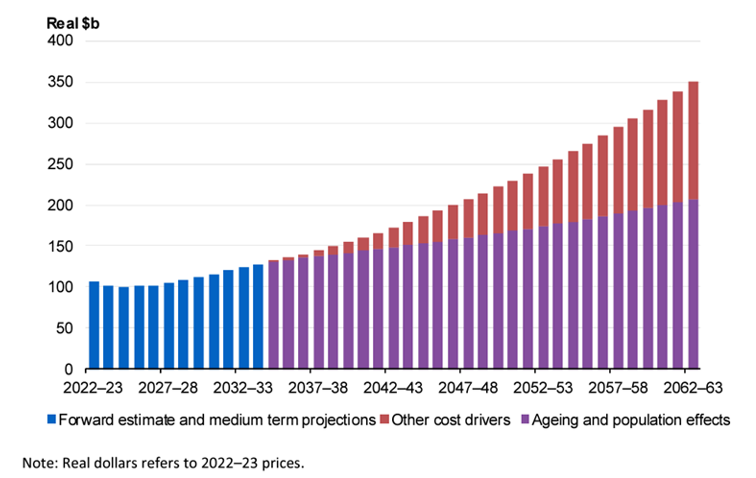
The longest timeline I have seen into the future is some Treasury modelling of health expenditure going forward for 40 years. But you can hardy call that a plan. You can find this modelling in the 2023 intergenerational report, and it shows a 250% increase in heath expenditure.
Chart 1: Australian Government Health Expenditure (Treasury)
If we were going to put together a 100-year plan for the human lifecycle, what should be some of our guiding principes?
- We would want to prioritise prevention (it’s a lot cheaper);
- We would want to support people’s preference to be managed in the community rather than in the hospital.
This 100-year plan would need to allocate funds to the various parts of the health system and would need to balance primary care and tertiary care, and balance prevention with acute care.
So, does the absence of a 100-year plan, or even a 30-year plan, mean that we just keep doing the same things decade after decade and we don’t see much fundamental change in the way our health system works?
You would think this might be the case. However, we see significant change, and the biggest change in the funding and the deployment of the medical workforce in the last 30 years has been the shift to hospitals.
Chart 2: Change in Australia’s medical workforce per 1000 people.
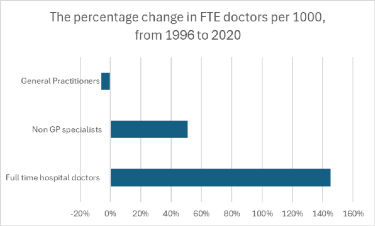
The percentage increase in hospital doctors per 1000 people over 25 years has been 145%, non-GP specialists have increased by 51% and at the same time the GP workforce is down 6%.
Another way of looking at this is that general practice in 1996 made up about 50% of the medical workforce and has declined to about 33%. Over the same time, hospital doctors have increased from 28% to 45% of the medical workforce.
Are governments aware this has happened and are planning to arrest the trend or possibly reverse it?
This is unlikely as Treasury is forecasting increases of 25% for Medicare and 35% for hospital care. Therefore, expect the trend to even higher levels of medical workforce allocation to the hospitals to continue.
The change in the medical workforce is not the result of planning. It is the result of a lack of planning and is tied to the short-term political election cycle that favours five-year plans. This driver favours acute hospital care rather than long-term preventive care.
What would Australia need to do to rebalance its medical system between GP-led primary care and hospital-based care?
It could be argued the “right” ratio of funding is probably something like 40% of the total health spend going to hospital care and 10% of total heath spend to GP-led primary care. That is a ratio of 4:1. Although the hospital spend is about 40%, the GP spend is a long way short of 10% — currently about 6.8% of the total heath spend.
Chart 3: Allocation of total health care spending
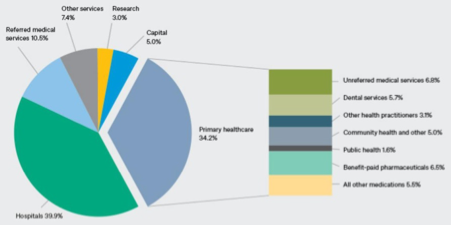
Australian GP-led primary care will need an additional $4 billion per annum to get to 10% of the total healthcare spend.
The usual refrain is there is not enough money.
However, an extra $4 billion per year is very achievable, and if the planning horizon is 10 years, then GP-led primary care will need to increase at 4% above the increase of hospital-based care.
For example, if hospital-based care funding increases at 6% per annum then GP care will need to increase at 10% per annum.
Whatever the increase, as long as the 4% gap is maintained then the funding ratio will be 4:1 in 10 years. If the goal is to close the funding gap over 20 years, then GP-led care will need to be 2% higher per annum than hospital-based care.
So, that’s one thing we would want to do in the first 10 or 20 years.
Now for the next 100 years.
Dr Hamish Meldrum is a GP and co-founding owner of the Ochre Health Group.