The inquiry already has ‘substantial support’ from within government and will look at unifying legislation across the nation to improve equity of organ transplant.
Assistant Minister for Health and Aged Care Ged Kearney has announced an inquiry into Australia’s human tissue laws, which were last reviewed in full almost 50 years ago.
In 1977, the Australian Law Reform Commission recommended an outline for human tissue legislation, that was subsequently adopted by all states and territories.
Over the years, amendments have led to the rise of inter-jurisdictional inconsistencies in the legislation, which have been outpaced by modern medicine.
The new ALRC inquiry will analyse the need for modernisation of the current laws and the possible need for harmonisation across all jurisdictions.
Attorney-General Mark Dreyfus said the inquiry already had “substantial support” from within the government.
“[A total of] 1396 Australians received a life-saving organ transplant in 2023 and thousands more had their quality of life dramatically improved by organ and tissue donations,” he said.
“There is strong support from states and territories for this inquiry to ensure our laws are brought up to date with the significant social, technological and scientific advances since Australia’s tissue laws were comprehensively reviewed in 1977.”
The inquiry will be jointly funded by the Commonwealth, state and territory health ministers, who are currently working to develop the terms of reference.
The commissioner for the inquiry has not yet been assigned.
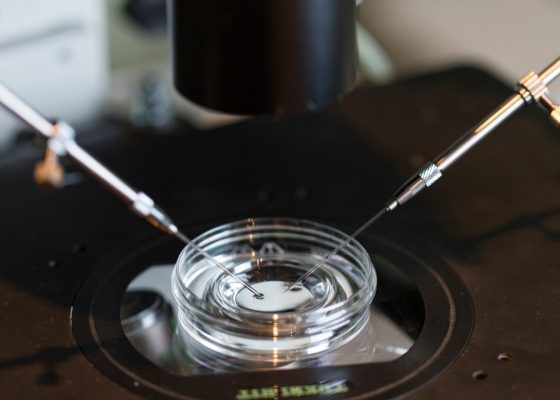
Transplant physician at Westmead hospital Professor Angela Webster told The Guardian that the current legislated definition of death was preventing the transplant sector from using novel medical organ retrieval technology normothermic regional perfusion (NRP).
Currently, in order for a person to qualify for organ donation they must be deemed dead as per the following definitions: irreversible end of blood circulation in the body or the end of all brain function.
Dr Webster said the definition should be updated to cessation of circulation to the brain, in line with most international medical definitions where NRP is used.
“As soon as circulation stops, organs start being damaged,” said Dr Webster, who is also a member of the board of the Transplantation Society of Australia and New Zealand.
“The idea of [NRP] is to stop the organ damage occurring by creating an artificial flow that allows oxygenation and allows tissues to stay healthy even though the person’s already dead.
“Because we’re establishing some circulation, albeit temporarily … that’s at odds with this definition of irreversible cessation of circulation of blood in the body.
“So there’s been concern we can’t use this technology in Australia because legally it is contrary to that definition of death.”
Dr Webster told The Guardian that standardising organ donation legislation across the nation would improve how successful transplants might be, thereby affecting equity.
“At the moment different things are permitted in different states, which might theoretically impact how successful a transplant is,” she said.
“And this shouldn’t be, and likely isn’t, the intent of the law. Organ donation and procurement should be uniform across Australia.”
The inquiry will involve public consultation, the dates of which have not yet been released.