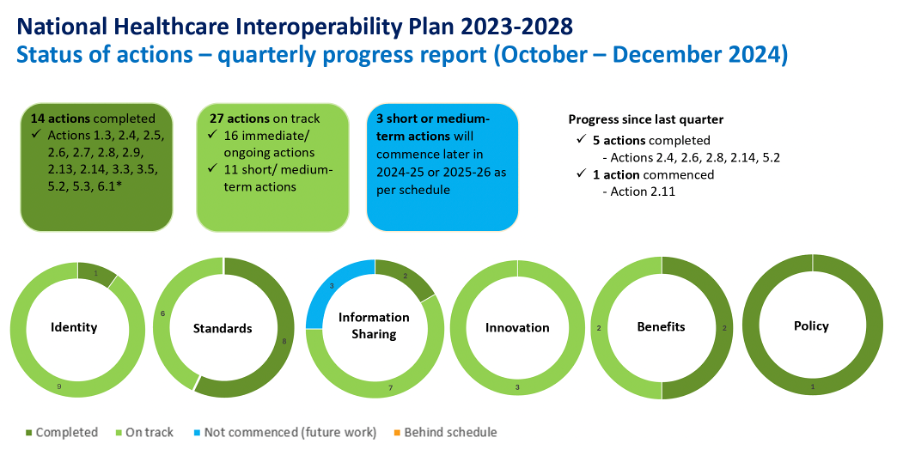
Although the ADHA is reporting it has delivered a third of the National Healthcare Interoperability Plan, there is a lot of devil in the detail of what is yet to be done for meaningful progress.
Chief digital officer of the Australian Digital Health Agency Peter O’Halloran hopped on LinkedIn yesterday to announce that of the 44 actions required to complete the National Healthcare Interoperability Plan 2023-28 the Agency has delivered 14 already.
“This is great progress, and we are only just getting warmed up,” quipped an enthusiastic Mr O’Halloran.
“I expect to see many more actions completed in the coming six months (ahead of the two-year anniversary of the launch of the Plan)”, he said.
But anyone looking at the latest quarterly update on the plan, published a few days ago, would immediately recognise that while 32% of the actions may have been completed, you probably couldn’t say that 32% of the work is done.
The key summary of what is actually done is produced below and most of it is policy and standards.
Policy, which was the vital first step, has been in place for a long time, thanks in large part to a lot of work on the part of the Department of Health and Aged Care, in co-operation with the Agency.
Standards are the vital second step because without a clear set of standards everyone can operate off there will be no alignment on technology and governance around interoperability and nothing will end up getting done.
What has been achieved in standards has been done in large part by the Sparked group at CSIRO in collaboration with the Agency. The Agency is reporting that standards are only 60% done, which is on schedule, but standards are the vital stepping stone without which not a lot in terms of technology alignment can meaningfully proceed.
Standards will need to be clear and be legislated in some manner or other soon, which is a fickle and often politicised process.
It’s also a process that a change of government could easily put a hard stop on if they don’t understand just how finely balanced and detailed the ADHA plans are.
Insider word is that the Opposition does not understand digital health priorities and plans very well at all. Everyone should probably also keep in mind that the last Coalition government had defunded the ADHA entirely in the budget forward estimates.
If you haven’t got time to read the whole quarterly update and want to judge progress on the green circles above, then the major circle of progress to be looking at is “Information Sharing”. It’s sort of the “everything in one” circle. Notably the dark green goes no where near 32% which might be the hint that we aren’t anywhere near one third done yet.
It’s mostly categorised as “on track”, which technically it likely is, but to get a lot more dark green (completed) into this circle, there are mass of individual and often highly technical projects that need to come together.
Put another way, there is a long, long way to go on a very complex journey here.
If you want to get a quick a sense of the devil in all this detail, look no further than what the Agency will need to bring to the table in terms of getting identity issues aligned across all the important points on the interoperability compass, including a so far low-key directory project called Provider Connect Australia (PCA).
The concept behind PCA is very sound: create a centralised single point of data upload portal, run through PRODA, for all providers in the country, which will distribute any additions or changes to provider details in the system across every meaningful point of provider engagement with the system and their key business partners.
Idealised, a working PCA would mean a GP, specialist, hospital or allied health provider, would enter a change or new addition details only once and those details would be automatically uploaded across the system at relevant points of engagement with key other providers and business partners, like, for example, the National Health Services Directory, major hospital networks (for more efficient discharge summary and e-referral delivery), PHNs, secure messaging providers, the major appointment engines and doctor directories, key practice business integrations like Cubiko (a practice and individual GP business data analysis application) or even Halo Connect, a rapidly emerging cloud based connector to the major provider patient management systems.
To make such a directory a reality is a lot of work which starts with getting lots of organisations aligned properly on identity – for this read the national health identifiers infrastructure.
Then the Agency has an interesting chicken-and-egg problem.
The idea of a one-time data entry and everything updates across the system should be a compelling proposition to every individual healthcare provider and their practice managers in the country.
But to be really compelling the Agency is going to need to populate the PCA with enough important business partners and other provider endpoints for the providers to care.
The PCA does already have a few good endpoints on board – Healthdirect’s National Health Services Directory, all the PHNs, some lower key secure messaging providers, and even eHealth NSW. But it needs a lot more and quickly to make a compelling case for the providers to take the time to register for the service.
The Agency is just now starting a marketing push on the PCA. It’s a great idea, but providers are a distracted and unforgiving bunch that is the archetypal herd of cats. They won’t appreciate or recognise at all how much work and technical smarts the Agency is paying for and working on to make the idea work, so the Agency is going to need to be very clever in its sell to get the idea across the line with key provider groups.
The PCA is just one example of devil and detail here, however.
A possibly oversimplified alternative to the “green circles” way to look at the giant amount of work the Agency, DoHAC and CSIRO are attempting here, is to think of the two key infrastructure projects in play that look like they are at the core of potential transformation in interoperability, and the precursors for these projects to succeed.
They are the rebooting of the My Health Record so it can share appropriate atomised records between providers and patients closer to real time, and the national Health Information Exchange.
The Agency hasn’t actually started on the technical reboot of the My Health Record yet, but it’s put the work out to tender, and it’s the logical first step because if it isn’t re-architected for cloud properly, all the data in it, and it’s role in interoperability so far (providers upload lots of patient data via e-PIP incentives and pathology is now being compelled to upload in near real time) won’t be usable in the greater scheme of sharing, much of which looks like it is going to hub around the national HIE.
All of this is not to say the Agency isn’t on actually on track or the plan is bad or isn’t working.
Technically the Agency is on track if you look in detail at what they said they’d do in what time, which is promising.
It’s just that announcing that you’ve completed one third of the actions of the National Healthcare Interoperability Plan might easily be construed by a lot of punters as we are a third of the way there to the sort of transformation interoperability vision outlined in the plan.
We may have done 32% of the actions, but there’s a good hard 95% of this – largely good – plan to get done yet, if, by 2028 we can all look back and say that the vision outlined in the plan looks like it will actually be realised.




