As in any fight, you need the right tools to succeed. It’s time to give all Australians with diabetes the same tools.
Australia’s diabetes epidemic is one of the largest and most complex health challenges we are facing as a nation.
More than 1.4 million (more than one in 20) Australians are living with diabetes. In the 12 months to March 2024, 115,000 people were newly registered with diabetes according to the National Diabetes Services Scheme (NDSS) – equivalent to 315 people newly registered every day.
Diabetes Australia estimates there are an additional 500,000 Australians currently living with undiagnosed type 2 diabetes.
That means that every day, the equivalent of a commercial planeload of people joins the growing number of Australians who now live with this condition.
At the Australian Diabetes Educators Association, our credentialled diabetes educators do exceptional work, helping to guide many people through this life-changing diagnosis. Diabetes is complex and unique to each person, and can require more than 180 decisions a day to maintain glucose levels within the person’s target range.
We know the challenge diabetes causes Australians every day – data from the Australian Institute of Health and Welfare shows that an estimated 1.2 million hospitalisations were attributed to diabetes in 2022. This means that more than one in 10 hospitalisations related to diabetes.
One thing that people with diabetes say to CDEs every day is that they don’t want to be in their GP waiting rooms, they don’t want to have to present to urgent care clinics, they don’t want to spend their nights in hospital emergency rooms.
They want to be able to manage their diabetes with support from CDEs, not add additional strain to an already overworked healthcare system.
Unfortunately, due to the cost-of-living crisis, many are now having to make decisions that will have long-term detrimental effects on their health.
In the lead-up to the 2022 election, the Australian public heard on several occasions from politicians that individuals were choosing between filling their prescriptions or buying groceries.
People living with diabetes in Australia are facing the same problem when it comes to the use of technology such as continuous glucose monitors.
As the name suggests, CGMs provide continuous glucose readings without the need for less accurate, older and painful methods such as frequent finger-pricking. CGMs consist of a wearable sensor that measures glucose data in real-time which is shared with a connected smartphone app. The app displays real-time glucose readings, generates reports for users and specialists, with some devices also offering customisable alarms to alert users to critical and potentially life-threatening low or high glucose events.
Thankfully the Australian government brought about a significant change on this front, delivering on their commitment for subsidised CGM devices for Australians living with type 1 diabetes.
To say this was a game-changing moment in the way diabetes is managed in this country would be an understatement. It has enabled greater support for those living with type 1 diabetes and CDEs now have access to the data to support these individuals through their daily challenges and to help them understand how to adapt their glucose management in response to changing circumstances throughout the day.
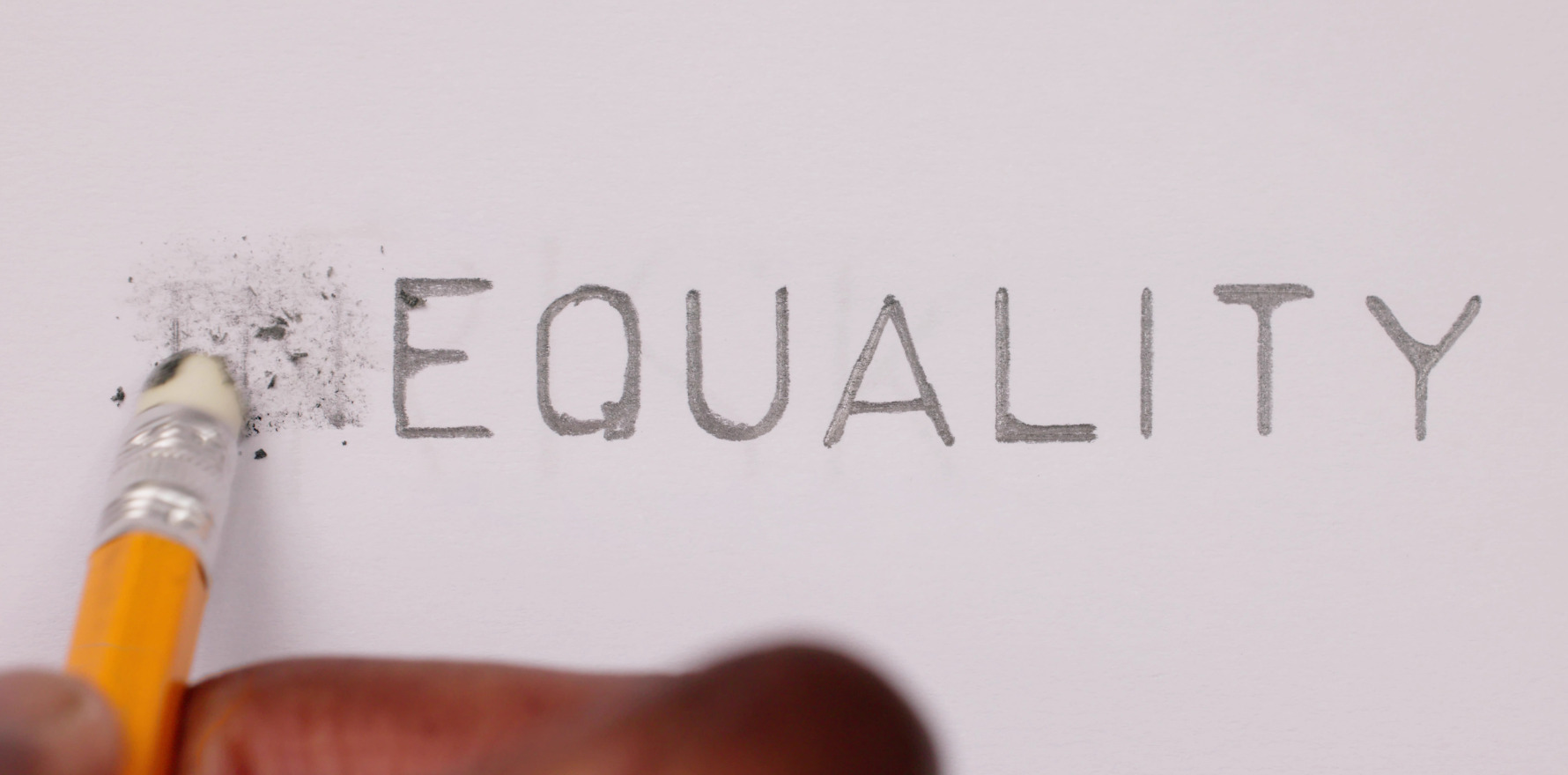
But for all the good this has done for those living with type 1 diabetes, it has created a perverse inequity in our system.
Australians living with type 2 diabetes and requiring insulin, as well as those living with gestational diabetes and requiring insulin, have no access to the subsidy.
This means that diabetes technology is only available to those who can afford the $4000 per year to access the technology which enables them to manage their diabetes well and minimise their risk of negative health impacts.
Many people cannot afford this expense. How is this possibly acceptable in a country like Australia?
Unless people with diabetes have access to the right tools and our CDEs have access to the right data, effective management of the condition will remain a pipe dream in Australia.
We estimate five hours of support in the use of diabetes technology is necessary to optimise technology use. This direct support may reduce the burden on our over-stretched GPs, as well as reduce emergency department presentations and hospitalisations.
It will help people living with diabetes to better manage their diabetes, reducing their glucose levels and the risk of diabetes-related complications in both the short and long term.
CDEs do invaluable work including pro bono and out-of-office hours to support the millions of Australians living with diabetes.
As in any fight, you need the right tools to succeed. Giving more Australians living with diabetes access to a subsidy will help them and their health professionals make the right decision at the right time.
We did not accept people choosing between filling a pharmacy script or buying their weekly groceries, and we should not accept people foregoing life-saving technology like CGM.
Susan Davidson is the CEO of the Australian Diabetes Educators Association.