The costings were not released due to the need for ‘comparative data’ relating to the cost of permanent staff, said DoHAC.
Locums may be essential to the medical workforce, but we need national collaboration to find a sustainable balance with permanent doctors, finds a Department of Health and Aged Care report, as locum costs rise.
The DoHAC has released an analysis of locum use in the medical workforce, based on a review by independent project consultant BDO.
The National Medical Workforce Strategy recommended an investigation into the higher costs of the locum workforce and the potential for fragmentation and operation outside of quality assurance systems.
“The situation worsened following the covid pandemic with increased demand for medical staff, increasing costs of locums and anecdotal concerns that more doctors were working as locums,” read the analysis.
The project, which started in May 2023, surveyed locums and other health professionals engaged with locums.
In total, 515 locum doctors and 380 non-locum doctors completed most of the survey questions.
Of the locum respondents, close to two thirds were GP or non-GP specialists, 17% were specialists in training and 17% were hospital non-specialists.
Around 25% worked as locums once or twice a year, while 17% were permanent locums.
The analysis recommended a review of the remuneration rates for permanent and locum roles and consideration of longer-term attraction and retention strategies.
It also recommended looking into improving the flexibility of employment options and workplace culture.
Only two jurisdictions, which were unnamed, supplied data on the cost of locums to the analysis. Both said the cost of employing locums was increasing.
Locum costs increased by 65% between the 2020-21 and 2023-24 financial years.
“The costs increased due to an increase in the number of locums, the cost per locum and the cost impact of the covid pandemic (costs increased and have not reduced to pre pandemic levels),” read the analysis.
“Insufficient information was available to provide a national view of locum costs.”
The analysis did not include the cost of locum doctors in the two jurisdictions as “comparative data is required to analyse the spend on locum recruitment versus the wages of permanent staff”.
The survey found that general practice, rural generalism, general medicine, emergency medicine, psychiatry and surgery had high locum use, which increased with remoteness.
The number one reason for choosing to be a locum was pay. This was closely followed by flexibility and autonomy.
Related
“If you … give them two options: permanent position – increased responsibility and accountability, more challenging workdays, reduced flexibility regarding workload/roster/leave; or locum position – reduced responsibility and accountability, less complexity/less challenging workdays, increased flexibility in regard to role/workload/roster/leave, more money per hour/day worked. How can we expect [doctors] to choose option one,” one survey respondent said.
According to the survey, reasons why a doctor might take a permanent job correlated with the reasons for choosing a locum position.

Almost 80% of locums surveyed would not have accepted a permanent position in their most recent role.
Poor work environment or mismanagement were identified by 23% of doctors as key barriers.
Some doctors suggested that, due to changing mentalities, more doctors would need to be trained compared to those retiring to maintain the same level of output.
“Train more doctors, taking into account that the new generations of doctors will work fewer hours and accept less afterhours work than those who are retiring. We need to train double the number of doctors than the number who retire,” said one respondent.
Some doctors said there was incongruence between training numbers and population distribution leading to limited progress or opportunities in their preferred specialty.
“Fix the career pathway, or fix the pay, because staff are clearly voting with their feet and losing permanent staff has long term negative consequences,” said another respondent.
Responses from other parts of the health system, such as those who engage locums, saw potential concerns with decreasing locum usage.
These included increasing pressure on the permanent healthcare team and disadvantaging practice reliant on locums.
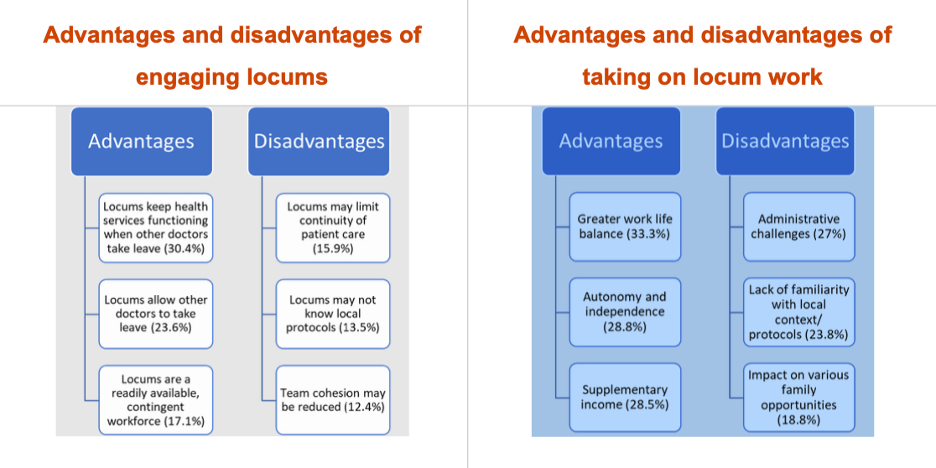
The analysis concluded that while locums were essential to the medical workforce, national collaboration was necessary to find the appropriate balance between locum and permanent doctors.
The analysis was limited by insufficient quantitative data, highlighting the need for better collection.
“BDO’s final report provided a useful understanding of the drivers of why doctors choose to locum and the locations and specialties that rely most heavily on locums.
“However, the survey results may not reflect broader locum workforce issues as respondents to the qualitative survey predominately identified as locum doctors,” read the report.




